
Chlorine Can Easily Cross the Dialyzer Membrane Causing
Chlorine, a commonly used disinfectant in dialysis treatment, plays a crucial role in maintaining water quality and reducing the risk of infection. However, there is a potential danger associated with chlorine when it comes into contact with the dialyzer membrane. During the hemodialysis process, chlorine can easily cross the dialyzer membrane and cause poisoning.
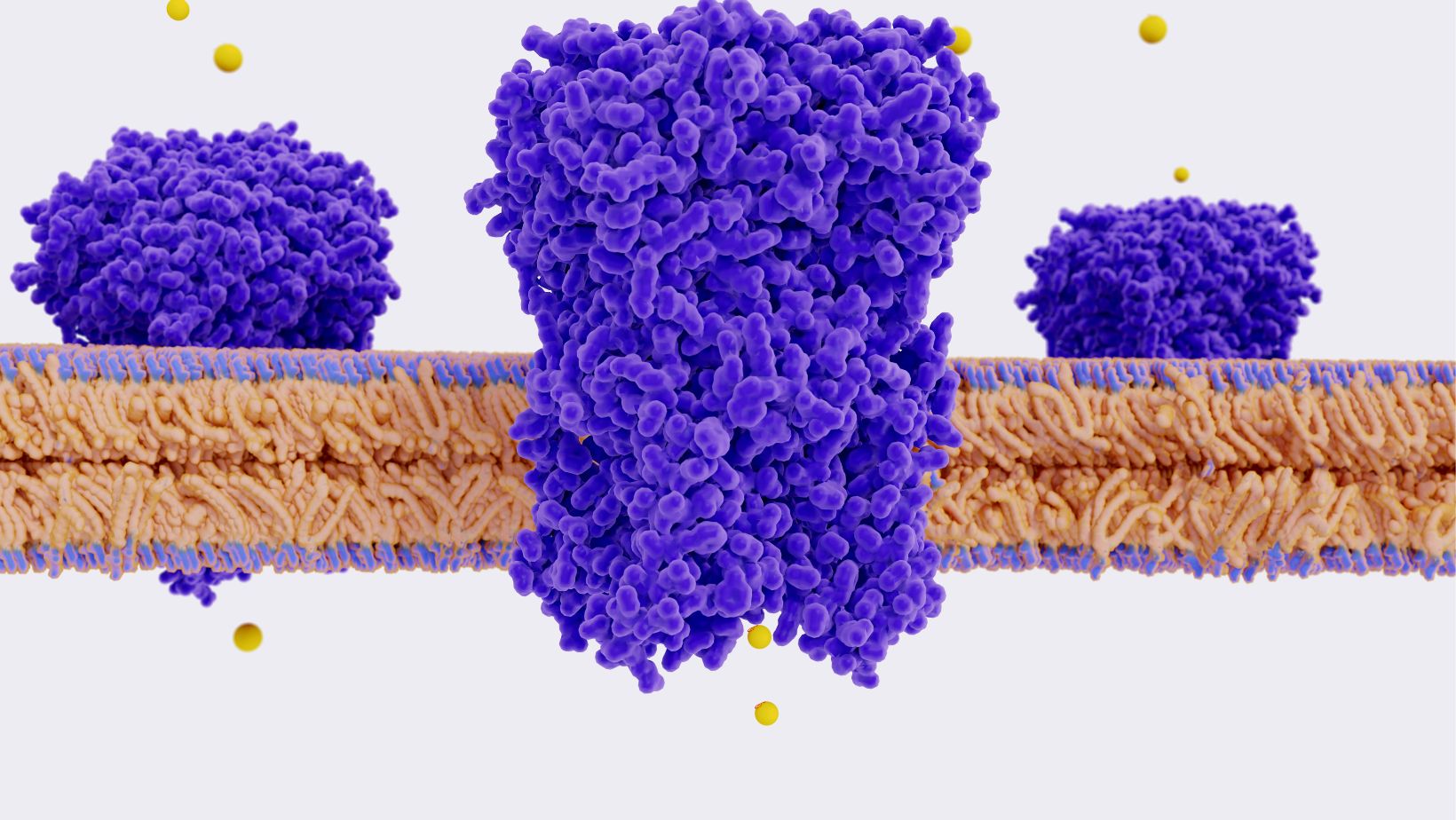
The dialyzer membrane acts as a barrier that allows waste products and excess fluids to be removed from the blood while preventing essential substances from being lost. However, this semi-permeable membrane is not completely impermeable to certain substances like chlorine. When high levels of chlorine are present in the water used for dialysis, it can pass through the membrane and enter the patient’s bloodstream.
Exposure to excessive amounts of chlorine during hemodialysis can lead to various complications such as respiratory distress, skin irritation, gastrointestinal problems, and even systemic toxicity. This highlights the importance of closely monitoring water quality and ensuring proper disinfection protocols are followed in dialysis centers.
In conclusion, although chlorine serves an important purpose in maintaining water safety during hemodialysis treatment, its ability to readily cross the dialyzer membrane poses a significant risk of poisoning if not properly controlled. Dialysis providers must prioritize regular testing of water quality and implement effective measures to prevent excessive chlorine exposure for patient safety.
What is Dialysis?
Dialysis is a life-saving medical procedure that plays a vital role in managing kidney failure. It serves as an artificial replacement for normal kidney function by removing waste products and excess fluids from the bloodstream. This procedure is necessary when the kidneys are no longer able to perform their essential functions effectively.
During dialysis, blood flows through a dialyzer, also known as an artificial kidney. The dialyzer consists of two compartments separated by a semipermeable membrane. One compartment contains the patient’s blood, while the other holds a special solution called dialysate. The semipermeable membrane allows small molecules like waste products and excess fluid to pass through it while retaining larger molecules such as proteins and blood cells.
There are two main types of dialysis: hemodialysis and peritoneal dialysis. Hemodialysis involves using a machine called a hemodialyzer to filter the blood outside the body, whereas peritoneal dialysis uses the lining of the abdomen to filter waste products inside the body.
Hemodialysis typically takes place at specialized centers where patients visit several times a week for treatment sessions lasting about four hours each time. On the other hand, peritoneal dialysis offers more flexibility as it can be done at home or even while traveling, allowing patients to have more control over their treatment schedule.
Both types of dialysis require strict adherence to dietary restrictions and fluid intake limitations to maintain appropriate electrolyte balance in the body. Additionally, regular monitoring of vital signs and laboratory tests is crucial to ensure that patients receive optimal care during their treatment.
In conclusion, dialysis plays a critical role in managing kidney failure by removing waste products and excess fluids from the bloodstream when natural kidney function becomes impaired. Whether through hemodialysis or peritoneal dialysis, this life-saving procedure helps improve patients’ quality of life and enables them to continue leading fulfilling lives despite their condition.
Why is Dialysis necessary?
Dialysis plays a crucial role in the treatment of individuals with kidney failure or severe kidney dysfunction. It serves as a life-saving procedure by effectively performing the vital functions that healthy kidneys would typically carry out. Here are some key reasons why dialysis is necessary:
- Waste Removal: One of the primary functions of the kidneys is to filter waste products and excess fluids from the bloodstream. When the kidneys are compromised, such as in cases of kidney failure, they cannot adequately perform this essential task. Dialysis steps in by mimicking this filtration process and removing harmful toxins and waste materials from the body.
- Fluid Balance: Maintaining proper fluid balance is another critical function of healthy kidneys. They regulate fluid levels by adjusting urine production according to the body’s needs. However, when kidney function declines significantly, excess fluid can accumulate in the body, leading to complications like edema or high blood pressure. Dialysis helps restore fluid balance by eliminating excess fluids through ultrafiltration.
- Electrolyte Balance: Kidneys also play a vital role in maintaining optimal electrolyte levels in our bodies, including sodium, potassium, calcium, and phosphate ions. Imbalances in these electrolytes can have serious consequences for various bodily functions and can even be life-threatening if left unaddressed. Dialysis assists in restoring electrolyte balance by selectively removing or adding specific ions to maintain equilibrium.
- Acid-Base Balance: The kidneys help regulate acid-base balance within our bodies by excreting hydrogen ions (acidic) or bicarbonate ions (alkaline). If this delicate balance gets disrupted due to kidney dysfunction, it can lead to metabolic acidosis or alkalosis—a condition that affects numerous physiological processes adversely. Dialysis aids in maintaining proper pH levels and preventing complications arising from imbalances.



